Developing biological drugs for inhaled delivery
Biological drugs have seen significant clinical and commercial success due to their high specificity and binding affinity, making these targeted therapies one of the fastest growing areas of the pharmaceutical industry. However, due to the low permeability and sensitivity to enzymatic degradation of these large, polar molecules in the intestine, oral delivery can be challenging. As a result, biotherapeutic agents are often administered by intravenous (IV) or intramuscular (IM) injection, creating a burden on patients who experience pain and inconvenience, particularly in the long-term treatment of chronic conditions1,2.
Inhalation offers an attractive, non-invasive route of administration for both local and systemic delivery of biologics. Lung delivery can be an effective means of treating various conditions, from pulmonary diseases such as asthma, COPD, cystic fibrosis, COVID-19 and other respiratory infections, which require a therapeutic to enter systemic circulation quickly, such as diabetes or migraine. By exploiting the large surface area and vascularisation of the lungs, as well as the high tissue permeability, pulmonary delivery can enable rapid absorption and fast onset of action. In addition to avoiding hepatic first-pass metabolism, the relatively low levels of proteolytic enzyme activity in the respiratory tract enables drugs to be absorbed readily into systemic circulation3.
However, the development of biomolecules into viable, efficacious medicines can often be challenging. Biomolecules can be sensitive to degradation when exposed external stresses which are common to pharmaceutical development processes, such as temperature changes (heating and cooling), pH, shear forces, mechanical agitation and light. In addition, the molecular characteristics of biomolecules must be carefully considered when selecting therapeutics for inhalation. For instance, properties such as charge can have in impact on the speed of diffusion through the lung mucus, influencing the rate of absorption and the rate of clearance. Generally, smaller proteins or fragments of antibodies achieve better tissue penetration and overall performance in the lung. Protein aggregation is another effect which must be carefully monitored, due to its potential implications on both therapeutic efficacy and immunogenicity2.
Manufacturing processes to produce dry, inhalable sized particles need to be identified which can harness the full therapeutic potential of a biologic, without sacrificing its potency. Crystec’s mSAS® (modified Supercritical Anti-Solvent) technology allows biomolecules to be processed in a relatively benign environment. Operating close to ambient temperature and eliminating exposure to surface tension and shear forces, mSAS® provides an attractive alternative to conventional technologies and offers the potential for improved retained activity, stability, and reconstitution. With the ability to buffer against transient acidity, incorporate additional agents (for stability or function) and titrate water into the composition of the particles where appropriate, further opportunities exist to retain structural and chemical integrity, promoting potency and stability, even at room temperature.
Crucially, mSAS® also offers the ability to engineer particles for inhaled delivery, by generating non-agglomerated, free flowing powders with a targeted particle size, which readily aerosolise. As a result, mSAS® particles can be efficiently deposited in the lung, delivering high therapeutic doses to the target site, even from simple inhaler devices. This efficiency of lung delivery can also result in lower dose requirements, reducing the cost burden of notoriously expensive biological agents. For systemic therapies, where large amounts of the drug have typically been required to achieve the necessary therapeutic levels, mSAS® provides opportunities to achieve impressive levels of lung deposition, even without the use of a carrier (e.g. lactose), further increasing the dose that can be achieved through inhalation.
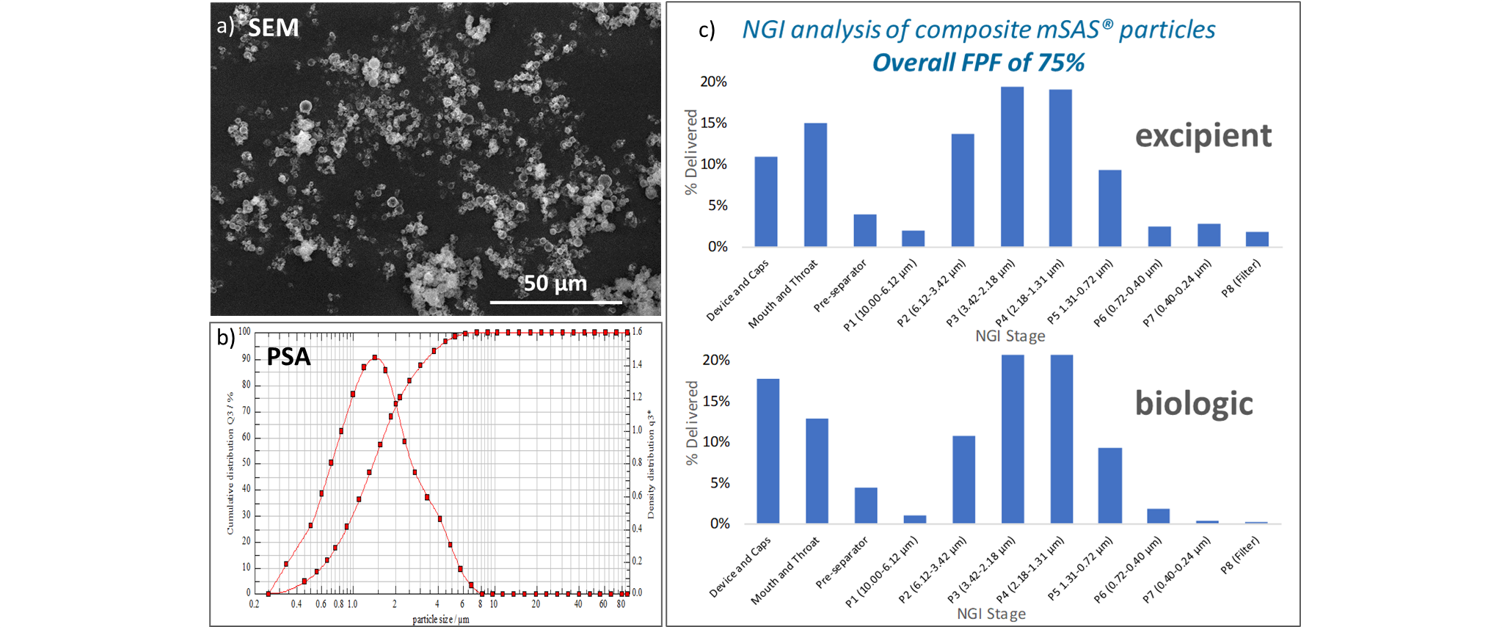
Conversely, many biologics are administered at very low doses. This can introduce a challenge in solid dosage forms, where the active must be blended with a bulking agent for the purposes of accurate dosing, which can result in process complexity and blend uniformity issues. By co-precipitating a regulatory approved bulking agent with the biologically active ingredient to generate mSAS® particles with a precise and uniform ratio of components, doses can be readily and reliably weighed into capsules for subsequent patient administration using a suitable inhaler device. Data shown in Figure 1 demonstrate the in vitro performance that can be achieved from mSAS® composite particles containing a low dose biotherapeutic and a dual-function excipient which acts as a stabilisation and bulking agent. This product prototype demonstrated retained activity in excess of 85%, with optimal particle size for deep lung delivery, a narrow particle size distribution, and a Fine Particle Fraction (FPF), of 75%. These data were found to compare favourably to recent data published for spray dried peptides, where FPF data in the region of 30 – 40 % were achieved4.
Figure 1: Analysis of mSAS® composite biotherapeutic by a) Scanning Electron Microscopy (SEM),b) Sympatec Particle Size Analysis (PSA) and c) Next Generation Impactor (NGI) studiesOverall, the delivery of biotherapeutics by inhalation offers immense potential to transform patient care, for both local and systemic effects, by reducing the need for invasive and painful injections. By applying Crystec’s mSAS® technology in the development of inhaled biotherapeutics, many of the challenges associated with the development of biologics can be overcome, from retaining potency and stability, to targeting desirable particle size and aerosolisation properties for efficient deep lung delivery.
References
1) Agu RU, Ugwoke MI, Armand M, Kinget R, Verbeke N. The lung as a route for systemic delivery of therapeutic proteins and peptides. Respir Res. 2001;2(4):198-209.
2) Liang W, Pan HW, Vllasaliu D, Lam JK. Pulmonary delivery of biological drugs. Pharmaceutics 2020;12:1025.
3) Labiris NR, Dolovich MB. Pulmonary drug delivery. Part I: physiological factors affecting therapeutic effectiveness of aerosolised medications. British journal of clinical pharmacology 2003;56:588-99.
4) Feliza M. Complex Biomolecules Analysis, Complex Biomolecules Require Analytical Evolution. Pharmaceutical Technology, Europe. 2021;33(7):26-28.
If you would like to learn more about Crystec and how the mSAS® platform can be applied to support the development of inhaled biotherapeutics, please get in touch directly at emily.bevis@crystecpharma.com.
To keep up to date with the latest news from Crystec, please follow us on LinkedIn.